
Smart use of artificial intelligence in health care Seizing opportunities in patient care and business activities
17 minute read
22 October 2020
For the health care industry, AI-enabled solutions can provide immediate returns through cost reduction, help with new product development, and lead to better consumer engagement. We explore how health care organizations can scale up their AI investments by pairing with a robust security and data governance strategy.
Executive summary
Artificial intelligence (AI) is already delivering on making aspects of health care more efficient. Over time it will likely be essential to supporting clinical and other applications that result in more insightful and effective care and operations. AI has multiple use cases throughout health plan, pharmacy benefit manager (PBM), and health system enterprises today, and with more interoperable and secure data, it is likely to be a critical engine behind analytics, insights, and the decision-making process. Enterprises that lean into adoption are likely to gain immediate returns through cost reduction and gain competitive advantage over the longer term as they use AI to transform their products and services to better engage with consumers.
Learn more
Explore the health care collection
Learn about Deloitte’s services
Go straight to smart. Get the Deloitte Insights app.
Deloitte conducted the State of AI survey in late 2019 which featured questions around how organizations are adopting, benefiting from, and managing AI technologies by industry. This survey was conducted before COVID-19 significantly impacted the United States. The survey found that:
- Health care organizations vary significantly in their AI investments: Seventy-five percent of large organizations (annual revenue of over US$10 billion) invested over US$50 million in AI projects/technologies, while approximately 95% of mid-sized organizations (annual revenue of US$5 billion to US$10 billion) invested under US$50 million. Seventy-three percent of all organizations expected to increase their funding in 2020.
- Top outcomes health care organizations are trying to achieve through AI are making processes more efficient (34%), enhancing existing products and services (27%), and lowering costs (26%).
- Respondents from health care organizations reported that their main concerns about risk with AI were the cost of the technologies (36%), integrating AI into the organization (30%), and implementation issues, including AI risks and data issues (28%).
The current pandemic overwhelmed health systems and exposed limitations in delivering care and reducing health care costs. The period from March 2020 saw an unprecedented shift to virtual health, fueled by necessity and regulatory flexibility.1 The pandemic opened the aperture for digital technologies such as AI to solve problems and highlighted the importance of AI. Even though the survey was fielded before the public health crisis, some of the outcomes and challenges that health care organizations had in using AI prior to the pandemic will likely continue to be instructive as health systems, health plans, and PBMs develop their new AI investment strategies.
Health systems were challenged by historic lower revenues due to nonurgent care and were forced to scale back during the pandemic. They can expect to gain advantage by using AI for applications to support cost savings as they transform.
Health plans and, in the longer-term, health systems, can use AI-enabled solutions to gain insights, develop new products and services, and better engage with consumers. Health plans can also use AI to proactively detect and manage fraud, waste, and abuse, resulting in recovered payments and cost avoidance, saving them millions and improving patient care.
This could well include an expansion of AI’s reach into clinical and back-office applications. Even as health care organizations step up their investments into data and analytics with AI, they should pair these with a robust security and data governance strategy.
Introduction
AI is gaining traction in health care, starting with automating manual and other processes, and the number of use cases and sophistication in the use of the technology is growing. In our vision of the Future of Health, we view radically interoperable data as central to the promise of more consumer-focused, prevention-oriented care, and analytics as critical to using the vast data that will be generated by ubiquitous sources. AI has already become embedded into analytics and is likely to become even more so in the future.
AI uses algorithms and machine learning (ML) to analyze and interpret data, deliver personalized experiences, and automate repetitive and expensive health care operations. These functions have the potential to augment the work of both operational and clinical staff in decision-making, reduce the time spent in administrative tasks, and allow humans to focus on more challenging, interesting, and impactful management and clinical work.
Today, health care organizations experience pervasive problems across their value chains, spanning every process on the continuum from care to cure. In the future, health care organizations that apply AI across every process from care to cure can improve the health and well-being of consumers. Deloitte’s Cognitive Care to Cure solution is an AI-powered, cloud-based, digital health care solution-as-a-service that can be applied across the health care value chain to improve operational efficiencies, reduce costs, and support better health outcomes for consumers (figure 1). These are all on the same platform and can offer efficiency to organizations looking for multiple solutions. They are also available as individual services, allowing health care organizations to choose from a menu of offerings that meet their needs and strategy.

Overview of AI
The term artificial intelligence is used for computer systems that perform human-like, mental tasks, such as visual perception, speech recognition, and decision-making based on data patterns. According to Deloitte’s Taking AI to the next level article, the key attributes of AI systems are:
- They learn. Unlike traditional computer systems that are programmed to follow a set of rules, AI systems get smarter over time and have the potential to deliver superior outcomes.
- Their core capabilities are like human intelligence. Pattern recognition, categorization, anomaly detection, and regression and prediction are good examples. AI can apply these capabilities to data sets and challenges that are far richer and more complex than those that humans can handle.
- AI is not just a single technology but a rich set of development techniques and problem-solving approaches.
Research methodology
Between October and December 2019, Deloitte’s Center for Technology, Media & Telecommunications surveyed 2,737 IT and line-of-business executives around the world to understand how organizations are adopting, benefiting from, and managing AI technologies by industry. Deloitte’s Center for Health Solutions analyzed the responses from 120 executives in health care organizations to understand the current and anticipated investments, top priorities, and AI risks and concerns related to health care organizations. Of these responses, 87 were from executives in US health care organizations while the remaining 33 were from regions including Australia, Canada, China, France, Germany, Japan, and the Netherlands.
We also interviewed a leader in a large national health plan to include insights on current applications of AI in that organization and what the future could hold.
Current applications of AI in health care
Health systems and health plans are likely to emerge from the response to COVID-19 with a renewed focus on efficiency and affordability. The American Hospital Association estimates US hospital revenue losses to increase by US$120.5 billion from July through December 2020, bringing total losses to around US$323 billion this year.2 Although health plans have remained financially buoyant through 2020, they are watching for economic trends that may result in more of their enrollees getting coverage through Medicaid and health insurance exchanges, which tend to pay less than commercial employers. Solutions that will deliver savings and efficiency have never been more relevant, and AI is embedded in many of these.

Increasing efficiencies and minimizing risks in clinical operations
AI-based solutions can effectively streamline diagnostic and treatment processes by using large amounts of structured and unstructured medical data across institutions. This can aid physicians at hospital and health systems in clinical decision-making by providing them with real-time, data-driven insights that they can alter and implement based on their personal expertise (see sidebar, “Improving patient outcomes with AI”).
“Health plans are utilizing the power of AI to make better predictions from data for external and internal stakeholders—proactively reaching out to consumers with information on disease progression and next best action for care, and supporting physicians in clinical decision-making by arming them with the right insights.”—Ashok Chennuru, Chief Data and Analytics Officer, Anthem Inc.
Improving patient outcomes with AI
- AI-based analytics for supporting the decision-making process: Researchers at the Mount Sinai health system recently developed an AI algorithm to rapidly detect COVID-19 by integrating patients’ chest CT scans with clinical information including symptoms, age, blood reports, and possible contact with infected people. The algorithm mimics the physician workflow used to detect COVID-19 and provides a final analysis using separate probabilities of CT images, clinical data, and both combined. The AI system also detected 68% of COVID-19-positive cases in situations where radiologists interpreted those cases as negative due to the negative CT appearance. The system can be effectively used to provide a second opinion to physicians and to triage or prioritize the evaluation of infected patients early in their admission to the emergency room.3
- Accelerating scientific discovery processes: AI health care company Imagia has collaborated with US and Canadian hospitals to accelerate health care discoveries through its EVIDENS platform. The platform empowers clinicians to structure data from live hospital systems by enabling automated data segmenting and labeling. It transforms unstructured clinical patient data into outcome-based structured information, thus scaling up traditional scientific discovery processes. The hospitals are working in collaboration to improve medical outcomes for lung cancer patients by analyzing treatments and results with the EVIDENS platform.4
AI-powered solutions can assist in accurately scheduling and planning clinical staff rotation—a major challenge for health systems since the onset of the pandemic—by factoring in operational constraints such as the number of staff, availability, skills, and specific equipment required (see sidebar, “Smart workforce management with AI”).
Smart workforce management with AI
- Norway-based Globus.ai’s AI-enabled system uses NLP, deep learning, and ML to extract information, match the competencies of health care workers to specific tasks, and help fill available slots, making the planning of medical staff rotation easier and more efficient. This has been saving hospitals 90% of the time it takes to fill each slot.5
- Deloitte’s smart workforce solution can help health care organizations realize workforce goals with the use of talent crowdsourcing (i.e., the gig economy). The solution provides clinicians with access to an internal crowdsourcing platform to complete activities, including top-of-license tasks, and uses AI-based analytics to optimize skill matching and workload requirements (internal clinical gig economy). The solution also supplements the traditional workforce with gig clinicians to complete routine activities during peak seasons and uses AI-based analytics to inform dynamic compensation for clinical services (external clinical gig economy). Core offerings include:
- Automatic resource allocation based on needs, historical preferences, and expertise across all in-network facilities
- Clinical and operational task prioritization based on urgency, including real-time reminders and progress tracker
- Efficiency solutions to reduce labor-intensive tasks through automation (e.g., patient scheduling, data exchange)
- Efficiency solutions expediting administrative burden (i.e., utilization management, prior authorization)
AI can also minimize patient risk by identifying medication errors that traditional rule-based clinical decision support systems are unable to detect, while also reducing alert fatigue and false positives—one of the reasons of physician burnout (see sidebar, “Minimizing safety risks through medication error detection with ML”).
Minimizing safety risks through medication error detection with ML
Israel-based MedAware's patient safety platform applies advanced ML algorithms and outlier detection mechanisms to identify and prevent medication-related errors and risks. The platform flags medications that conflict with the profile of the patient, physician, or institution. MedAware flagged 10,668 potential errors and adverse drug events in the records of 373,992 patients treated in the outpatient clinics of Massachusetts General and Brigham and Women’s Hospitals. In an analysis done on a random sample of 300 warnings generated by MedAware, 92% of the warnings were accurate based on data available, 79.7% of the warnings were clinically valid, and 68.2% of the warnings would not have been flagged by existing decision support systems.6
Increasing efficiencies and enhancing customer experience in nonclinical operations
The ability of AI to examine large amounts of information quickly can help hospital and health plan administrators optimize performance, increase productivity, and improve resource utilization, resulting in time and cost efficiencies. Additionally, AI-enabled solutions can speed up and strengthen the insight generation process by allowing the organization to gain the holistic picture it needs to make data-driven decisions. Finally, AI can also deliver personalized experiences by facilitating conversations with patients through virtual assistants (see sidebar, “Optimizing nonclinical operations with AI”).
Optimizing nonclinical operations with AI
- Achieving time and cost savings by automating administrative tasks: Ohio-based Olive’s AI Workforce solution is designed to automate a selection of tedious, high-volume administrative tasks in various departments of a health care organization such as revenue cycle. Olive uses ML to find patterns among its data feeds, allowing the tool to identify workflows and processes suitable for optimization. To date, Olive has completed over 450,000 claim status checks and processed more than 250,000 charge corrections for its clients.7
- Accelerating and amplifying insights generation: HealthcareX is a self-service platform with analytics, AI, and visualization capabilities developed by Deloitte to accelerate and amplify insight generation for health systems and health plans. HealthcareX can be used to federate data from multiple sources to one location, remove manual data collection processes, standardize data using preset functions to ensure data integrity, uncovering and exploring connections in data, and creating tailored insights. This eliminates the need for multiple systems and allows the organization to enhance the decision-making process. An application of the HealthcareX tool is to analyze member population to predict high-cost claimants for health plans.
- Enhancing customer experience through conversational AI: The COVID-19 pandemic has led to patients making more phone calls and rapidly adopting virtual health, exposing the limitations of health systems. This has set the groundwork for a digital front door. Deloitte’s DocTA is an omnichannel experience powered by conversational AI integrated at the contact center to resolve administrative inquiries and steer consumers to appropriate endpoints of care.
According to the Journal of the American Medical Association (JAMA), approximately 25% of US spending on health care is wasteful, translating into an estimated US$760–935 billion wasted every year.8 However, AI-based analytics present the opportunity for health plan companies to detect and reduce improper billing practices for streamlined member billing. Additionally, PBMs can use AI to integrate and assess patient medical information to resolve issues in real time, leading to improved patient care experience. AI can also help to effectively and proactively identify potential fraud, waste, and abuse (see sidebar, “Realizing efficiency through fraud, waste, and abuse [FWA] detection and prevention”).
Realizing efficiency through fraud, waste, and abuse (FWA) detection and prevention
- Deloitte Risk and Financial Advisory’s Program Integrity solution is an end-to-end solution that integrates and analyzes provider claim data using ML models to develop comprehensive analytics for the identification of potential fraud and improper payment. The solution continues to support a large national health plan in reducing improper payments through various initiatives, one of them being by creating a data-driven advanced analytics anomaly detection solution that applies ML techniques to existing data to uncover risks and provide an enterprise view of hidden behaviors and trends across all lines of business.
- Prime Therapeutics, a PBM, is using an AI solution to identify FWA, assisting health plans with cost savings and improving patient care. The AI platform integrates pharmacy and medical claims data from prescribers, pharmacies, and members. Investigators can link a patient’s prescriptions to a diagnosis and associated medical visits, and also monitor for drug overutilization. The company has saved US$355 million in recovered payments and cost avoidance for health plans since mid-2018.9
Current and anticipated investments, top priorities, and risks and concerns with AI
Interest in AI in health care has surged since last year as provider and payer organizations seek to tap the potential benefits offered by data-driven analysis and deep neural networks.10 Clinicians are more open to digital technologies, since they experienced firsthand during the pandemic how these technologies augmented their skills in areas including surgery and diagnosis. As these organizations begin to scale up their AI applications based on their short- and long-term priorities, they should be mindful of risks during implementation.
AI investments in health care vary widely; payback period is in line with expectations
Surveyed leaders agreed that health care organizations are investing, but the investments vary widely. Seventy-five percent of large organizations (annual revenue of over US$10 billion) invested over US$50 million in AI projects/technologies, while approximately 95% of mid-sized organizations (annual revenue between US$5–10 billion) mostly invested less than US$50 million (figure 3). Seventy-three percent of these health care organizations also expect their investments in AI to increase in the next fiscal year.11 Additionally, most of the surveyed leaders believe that the actual payback period for their organization’s AI investments is in line with their expectations.12

Top priorities include increasing process efficiency, enhancing customer offerings, and lowering costs
AI has the potential to create new efficiencies in administrative processes and provide a precise and faster diagnosis and treatment plan for each patient, resulting in reduced length of stay, fewer subsequent readmissions, and reduced costs.
When asked about the outcomes organizations are trying to achieve through AI, surveyed health care leaders cited more efficient processes as their top priority (34%). Enhancing existing products and services (27%) and lowering costs (26%) are a distant second. None of these organizations has achieved all outcomes to a great extent, but making processes more efficient comes the closest (43%) (see figure 4).
Another Deloitte survey, conducted in February 2020 and with a focus on physicians, had similar findings. Seventy-three percent of the surveyed physicians reported that saving time and resources is expected to be the No. 1 benefit of AI. Additionally, over 50% of surveyed physicians said they would increase their use and support of AI-driven solutions if they are shown to improve efficiency and quality.13

Top challenges include cost of AI solutions, AI integration problems, and AI implementation, data, and risk issues
Survey respondents pointed to poor-quality data, siloed data systems, high initial costs of AI solutions with low return on investment, and integrating AI into legacy systems as concerns.

Surveyed leaders indicate that the top challenges faced by their organizations include cost of systems (36%), integrating AI into the organization (30%), and AI implementation, data, and risk issues (28%) (see figure 5).14 When asked about ethical risks, they mentioned that they were most worried about safety concerns around AI-powered systems (28%).15 Additionally, findings from the 2020 Survey of US Physicians indicate that 69% of the physicians are concerned about who is liable when AI-driven solutions make a mistake.16
Risks and trust framework
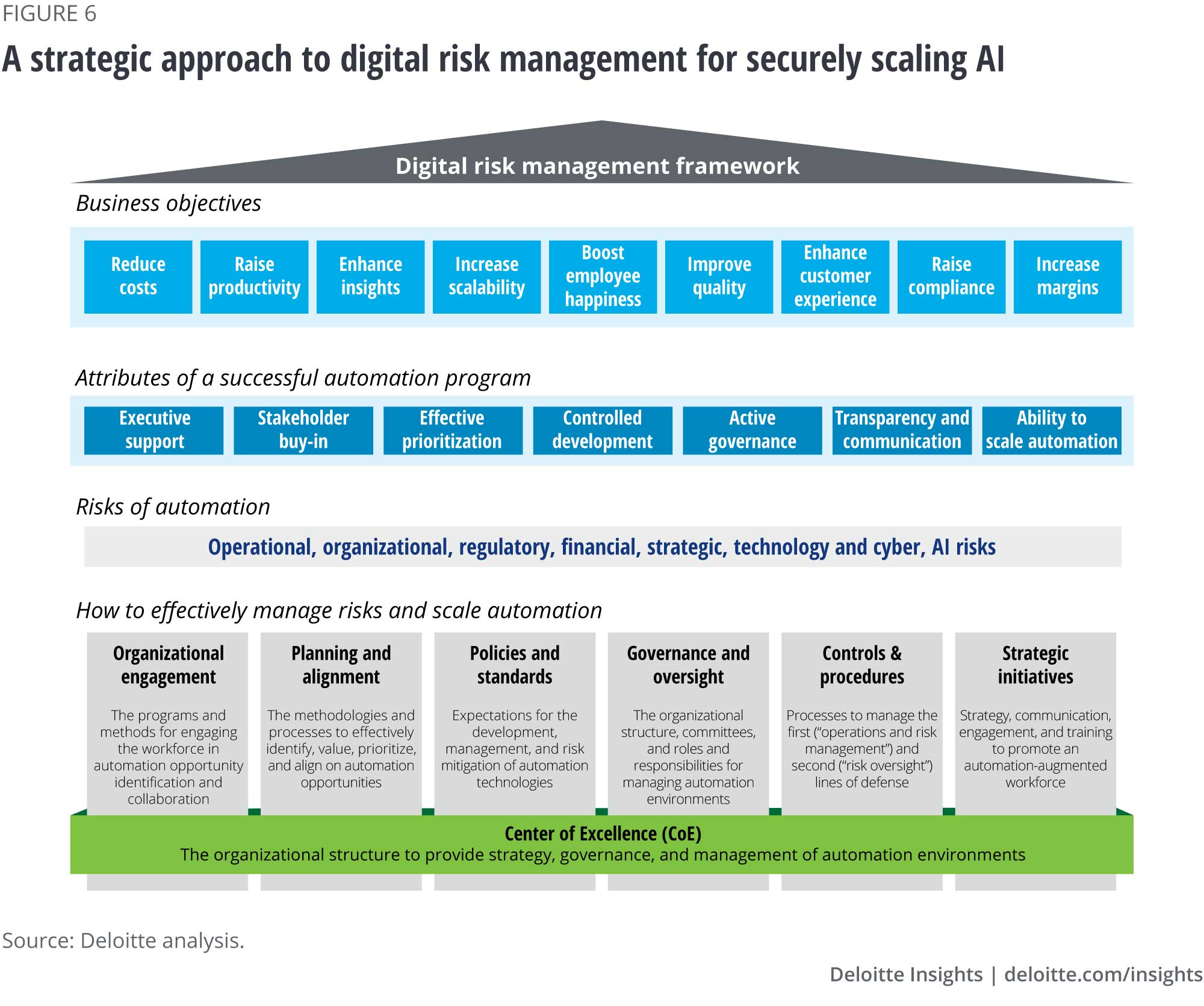
As investments in AI increase and AI-powered solutions become more widespread in health care settings, the industry should address the new set of challenges both from the data used—including cyber threats—and the potential for bias in the AI algorithms. The strategy should comply with regulations—including to assure patient privacy and other HIPAA requirements (figure 6).
AI algorithms present risks such as variability of output in patient diagnosis and treatment, data bias, and traditional IT risks such as change management. Health care organizations should verify the integrity and accuracy of their AI algorithms by focusing on:
- Data strategy: Organizations should start incorporating inclusivity, equity, and fairness into the data collection process, training and testing of AI algorithms equally well across different geographical regions. They should also conduct an internal audit and testing for AI systems and ensure that AI vendors provide unbiased systems. Understanding the data strategy and process is critical to minimizing bias in the AI model.
- Testing: Testing of ML or cognitive algorithms doesn’t fall into the traditional test case construct where the actual results can be compared to an expected result repeatedly with the same outcome. Learning algorithms will produce varying outputs each time they learn. Organizations should think about testing data differently.
- Monitoring: Because learning algorithms adjust to new data over time, what they learn should be monitored to ensure it stays within the acceptable control limits. This is a critical component for maintaining validation and compliance in the operational state.
For health systems and health plans to achieve their business objectives, they should:
- Ensure multistakeholder buy-in on validating the entire AI life cycle and the organizational/human processes that surround the AI system.
- Ensure strong governance practices around AI to enable organizations to innovate with confidence while reducing the risks that come with complex technology.
- Ensure patient data privacy and protection from cyber threats by addressing all kinds of risks—external, physical, and digital, among many others—and assess whether the potential benefits sufficiently outweigh the associated risks.
- Include policies that clearly establish who is responsible and accountable for the AI output. Key factors to consider include which rules and regulations might determine legal liability and whether AI systems are auditable.
- Ensure transparency by informing the consumers how their medical data is being used by AI to make decisions. AI’s algorithms, attributes, and correlations should be open to inspection, and its decisions should be fully explainable.
Implications, call to action
AI is delivering significant business benefits today—and its potential to shape the future of the health care industry is even greater. Health care organizations that are still in the experimental pilot phase stand to be left behind by payers and competitors.
“It is essential for health care organizations to understand how to automate processes by reimagining them. That’s where AI can help. The ‘digital-first, AI-first, insights-driven organization’ mindset needs to be incorporated into every business unit of the enterprise with a focus on automation.”—Ashok Chennuru, Chief Data and Analytics Officer, Anthem Inc.
For health systems: To prepare for the Future of Health, health systems should move from the experimental stage to having data and advanced AI as a core capability.
Health systems are currently under a lot of financial stress. For them, the short-term focus might be on investing in AI approaches that will help them achieve cost savings. Some examples of these are provider profiling (supply chain); fraud, risk, and abuse detection and prevention; and automating health care operations.
Over the longer term, health systems can invest in more transformative AI applications to improve their competitive positioning, achieve profitable growth, engage consumers, and deliver personalized customer experiences. Health systems should actively cultivate their relationships with AI start-ups, technology and professional services firms, and academia, and consider taking a more active role in AI innovation. They should also encourage stakeholders, including physicians, clinical staff, and administrative staff to strive to be champions and promote an AI-augmented workforce.
For health plans: Some health plans are already investing deeply in data and AI-based analytics. The focus should be to use AI to improve health insurance cost-efficiency, consumer engagement, insights for medical and organizational management, and client outcomes, to complement the company’s overall positioning and strategy.
For PBMs: PBMs need to focus on determining and improving communication channels with health plans and use AI to optimize staffing and distribution activities. They should invest in AI to enable proactive management resulting in effective savings programs and pharmacy programs designed to improve the patient journey.
As all health care organizations figure out how to scale up AI-led innovations, they also should manage AI’s unique risks. Deloitte’s Trustworthy AI framework can help health care organizations identify and manage AI risks effectively to enable faster and more consistent adoption of AI.
More on health care
-
Building resilience during the COVID-19 pandemic and beyond Article4 years ago
-
Improving care and creating efficiencies Article4 years ago
-
Loss of health insurance from the pandemic Article4 years ago
-
Virtual health care Video
-
Medicaid in 2040 Article4 years ago
-
The future of virtual health Article4 years ago
















