But the health funding database Rock Health noted that changes in business models, increased focus on direct-to-consumer and even business-to-consumer-to-business, as well as infrastructure and talent pools, may have the biggest impact on the sector moving forward.5 Venture capitalists, private equity, health care organizations, and other investors have already begun investing in startups that call themselves platforms. For example, veda, an AI-powered data-processing platform that uses smart automation to streamline health care administrative tasks, raised US$45 million series B funding led by Oak HC/FT.6 Digital health company b.well raised US$32 million in its series B fundraising round to drive its next development phase, led by HLM Venture Partners.7 b.well gathers patient data across providers, insurers, pharmacies, and a patient's own apps and devices, and enables consumers to navigate through their own care journey. Disease-specific platforms are also generating interest; Khosla Ventures has invested in both Alzheimer’s disease (Neurotrack’s series C funding) as well as cell therapy (Cellino seed investment and series A funding). IVF (TMRW Life Sciences equity round, led by Transformation Capital) and autoimmune diseases (Drugviu seed funding from Avestria Ventures, Cleveland Avenue, and ImpactAssets, among others) are other areas of interest.8 Transcarent, which was evaluated at US$1.62 billion in January 2022, making it the latest digital health unicorn,9 is a “comprehensive, consumer-directed health and care platform for employees of self-insured employers and their families.”10 Investors see potential in this space as platforms such as Transcarent can “address the challenge [of health care] in a new and different way that is focused first and foremost, on the consumer.”11
Of the nine health care startups that went public in 2021, four describe themselves as platforms.12 But not all startups that call themselves a platform will be successful. The markets will distinguish between those that are true platforms and those that are not, and value them accordingly.
What are platform businesses?
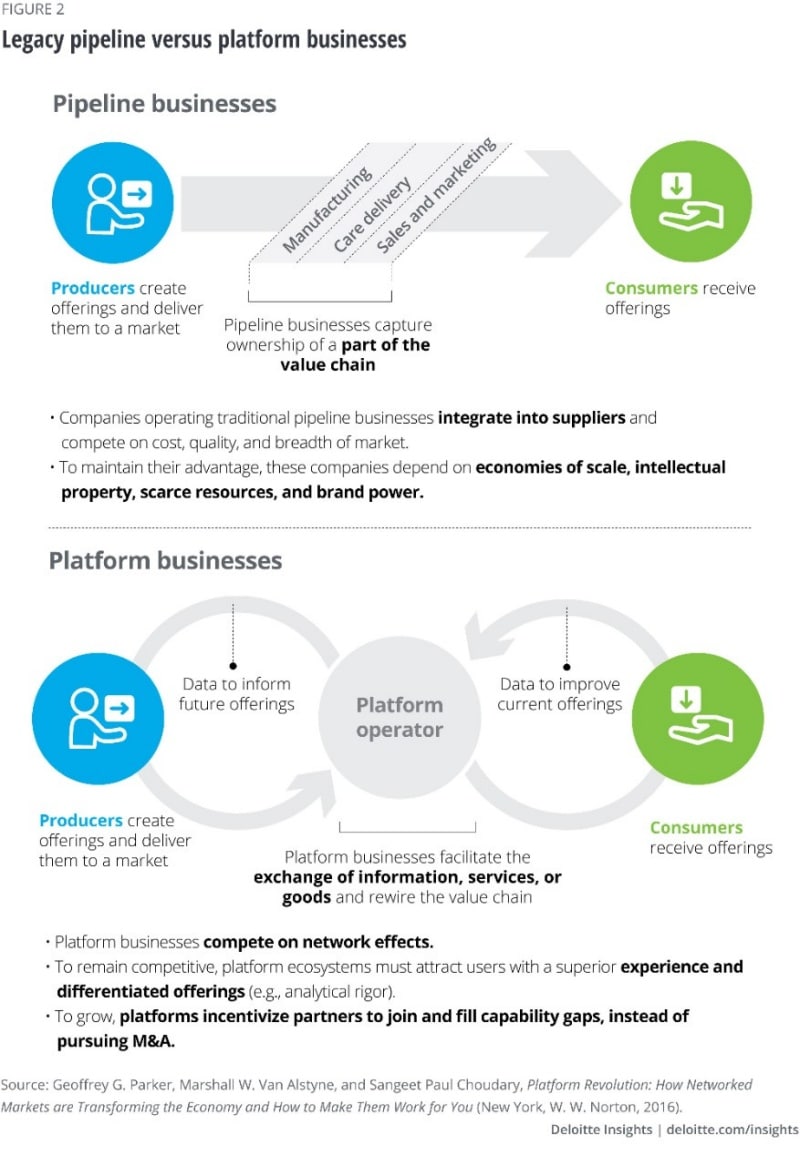
Many health care organizations have traditionally relied on M&A to grow or diversify, either as an opportunity (e.g., increase market share) or to mitigate threats (e.g., changing reimbursement models). However, M&A may not always be the best option due to constraints with capital, talent, and organizational structure. Technology advances in the past few years have enabled health care organizations to achieve similar ends (growth and diversification) through a newer avenue—platform-enabled ecosystems—paving the way for transforming traditional business models.
Ecosystem conveners create a platform that aggregates goods and services provided by ecosystem partners. In industries such as retail, entertainment, and hospitality, such business models have rewired value chains by providing a better, digitalized customer experience while making suppliers more accessible—in turn, attracting more and more participants onto the platform (figure 2).